Gingivitis is one of the most common dental problems in the world, but many people are surprised to learn that it does not always affect the entire mouth at once. Sometimes, patients notice swelling, redness, or bleeding around only one tooth and wonder if this means they have gingivitis in just that specific area. Understanding whether gingivitis can appear around a single tooth and why it happens is extremely important because early treatment can stop the condition from spreading. Gum disease always begins as mild inflammation, and catching it early is the key to protecting long-term oral health. In this complete guide, you will learn everything about how gingivitis starts, why it can appear around only one tooth, how to reverse it, how to prevent it, and when to seek professional help.
Gingivitis is an inflammation of the gums caused by harmful plaque bacteria. These bacteria stick to the gumline and produce toxins that irritate the gum tissue. While many people think gum disease always affects the whole mouth, the truth is that gingivitis can easily develop in one small area, especially when there is plaque buildup, food trapping, a tight dental contact, misalignment, or poor cleaning habits in just that spot. This means it is completely possible to have gingivitis around one tooth while the rest of your gums look normal. Understanding this helps you take proper action quickly before the inflammation spreads to other teeth or becomes a more serious form of gum disease.
What Is Gingivitis?
Gingivitis is the earliest stage of gum inflammation, and it is almost always caused by plaque. Plaque is a soft, sticky film made of bacteria, food debris, and saliva. If not removed daily, it hardens into tartar, also called calculus, which is even more irritating to the gums. When plaque and tartar stay around the gumline, the gums become red, swollen, and tender. The first sign is usually bleeding during brushing or flossing. At this stage, the condition is reversible because it has not yet affected the bone or deeper tissues.
The gums around a healthy tooth should be pink, firm, and tight. When gingivitis develops, the gums begin to look puffy, shiny, or darker in color. They may feel sore when touched or start bleeding easily. Many people think that bleeding gums are normal, but this is actually an early warning sign that the body is trying to fight inflammation. The good news is that since gingivitis is the mildest form of gum disease, proper care can heal it completely. Understanding the early signs helps prevent more serious conditions like periodontitis.
Can Gingivitis Affect Just One Tooth?

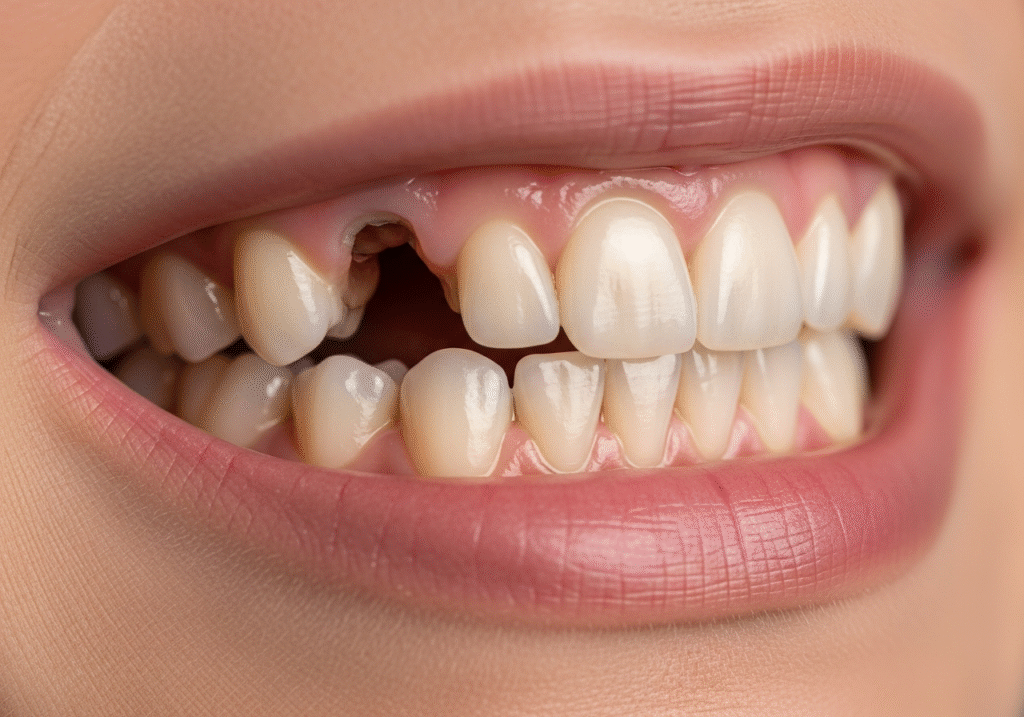
Yes, gingivitis can absolutely affect only one tooth. This is called localized gingivitis, and it is extremely common. Many people are surprised because they assume gum disease affects the whole mouth at once. But the truth is that plaque does not spread equally on every tooth. Sometimes, one area becomes harder to clean due to crowding, a cracked filling, or a spot where food easily gets trapped. As a result, plaque collects more on that specific tooth, leading to inflammation only in that one area.
Localized gingivitis can also happen if someone brushes unevenly. People often brush their dominant side more thoroughly and unintentionally neglect the opposite side. In some cases, only one tooth is misaligned or rotated, making it harder to clean. A single tooth can also develop gingivitis if it has a deeper pocket or if gum recession exposes more surface area for bacteria to stick to. This makes the condition very easy to isolate. Understanding localized gingivitis is important because early treatment prevents it from becoming generalized disease.
Early Signs of Gingivitis Around a Single Tooth
When gingivitis affects only one tooth, the symptoms appear only in that specific area. The gum around the tooth may become red while the gums around the other teeth remain pink. The affected area might bleed when flossing, especially if the tooth is at an angle or if the gum pocket is deeper than usual. You may feel soreness or tenderness when touching the gum or chewing food on that side. Sometimes, the tooth may feel slightly loose because inflammation weakens the supporting gum tissue.
A bad taste or mild odor can also occur if food particles become trapped around that tooth. The gum may appear more swollen compared to others, and you might notice a slight throbbing sensation. These symptoms are usually mild, but ignoring them can lead to something more serious. Catching these early signs is key because early treatment is easier and faster.
Causes of Gingivitis in One Area
Localized gingivitis can occur for several reasons. One of the most common causes is poor oral hygiene in that particular spot. If a person skips flossing or misses the same tooth repeatedly while brushing, plaque will begin to build up. Crowded or overlapping teeth also collect more plaque, especially if the toothbrush bristles cannot reach the gumline properly. Dental restorations like crowns or fillings that do not fit well can trap food and bacteria, increasing the risk of inflammation in that small area.
Lifestyle habits also contribute. Frequent snacking, mouth breathing, and dehydration can cause the gum around a single tooth to dry out, making it easier for bacteria to attach. People who clench or grind their teeth may irritate the gum around one tooth more than others. Even using toothpicks aggressively can injure the gum and create a space where bacteria thrive. Because so many small factors can cause localized gingivitis, it is important to identify the exact reason for proper treatment.
How Localized Gingivitis Develops
Localized gingivitis develops slowly at first. It begins when plaque settles at the gumline of one tooth. Without removal, the plaque bacteria multiply rapidly. The toxins they release irritate the gum, making it swollen and red. Continued irritation causes bleeding, especially during brushing or flossing. As inflammation increases, the gum may pull slightly away from the tooth, creating a small pocket.
This pocket becomes a perfect hiding place for more bacteria, making the condition worse. If tartar has already formed, it creates a rough surface that attracts even more plaque. Over time, the gum around the tooth becomes more inflamed. Without treatment, this can eventually lead to periodontitis, a more advanced stage of gum infection that involves bone loss. Fortunately, early localized gingivitis is reversible, and proper care can stop the disease before it becomes serious.
Risks of Ignoring Gingivitis in One Tooth
Ignoring gum inflammation, even if it affects only one tooth, can lead to serious consequences. Inflammation can spread along the gumline to nearby teeth. The plaque that caused the initial problem can easily move to other areas if oral hygiene does not improve. If gingivitis becomes chronic, the gum may start to recede, exposing more of the tooth’s root. This leads to sensitivity and increases the risk of cavities.
Eventually, if left untreated, localized gingivitis can turn into localized periodontitis, which involves bone destruction. This can cause the affected tooth to loosen and eventually fall out. Once bone is damaged, it cannot grow back naturally. This is why dentists emphasize early treatment.
How Dentists Diagnose Localized Gingivitis

A dentist diagnoses localized gingivitis by examining the gums carefully. They look for redness, swelling, and bleeding around the tooth. They may gently probe the gum pocket around the affected area to measure its depth. Healthy gums usually measure around one to three millimeters. A deeper reading around just one tooth indicates localized inflammation.
Dentists may also check for tartar buildup, misaligned teeth, or faulty dental restorations. If food trapping is present, they will identify the cause. X-rays may be taken to make sure the bone around the tooth is still healthy. All this helps the dentist create a proper treatment plan.
Treatment Options for One-Tooth Gingivitis
Treatment depends on the cause of inflammation. The dentist will begin by cleaning the affected area thoroughly. They will remove plaque and tartar using professional instruments. If a restoration is trapping food, they may reshape or replace it. If the gums are irritated due to a rough surface, the dentist will smooth it out.
Sometimes, a special cleaning called scaling is needed to remove tartar from deeper pockets. Antimicrobial rinses may be recommended to reduce bacteria. For some patients, correcting crowding or improving flossing technique is the key to preventing recurrence. With proper treatment, localized gingivitis usually heals within days or weeks.
Home Care Steps to Reverse Early Gingivitis
Daily home care is essential. Brushing twice a day with soft bristles removes plaque. Flossing removes debris trapped between teeth. For localized gingivitis, focusing on the affected area is important. Warm salt water rinses help reduce swelling and kill bacteria naturally. Drinking more water helps maintain saliva flow, which protects gums.
Some patients benefit from using an electric toothbrush because it cleans more effectively. Others may need interdental brushes if the tooth has a wider gap. Improving oral hygiene habits ensures faster healing and prevents the condition from spreading.
How Long It Takes to Heal Gingivitis in One Tooth
If caught early, gingivitis in one tooth can heal within a few days. Proper brushing, flossing, and rinsing can significantly reduce inflammation quickly. However, if tartar has built up, healing may take one to two weeks after a professional cleaning. If gum pockets are deeper, full recovery may take several weeks.
Healing time also depends on habits. Smoking, poor diet, or inconsistent hygiene can delay recovery. A healthy lifestyle and proper cleaning speed up healing dramatically.
Can Gingivitis Spread from One Tooth to Others?
Yes, it can spread. If plaque is not removed regularly, it can move to nearby teeth. Bacteria multiply rapidly and can travel along the gumline. This means localized gingivitis can become generalized gingivitis over time. Early treatment prevents the condition from affecting more teeth or turning into periodontitis, which is much harder to treat.
Taking care of the affected tooth immediately is the best way to prevent spreading. Good daily hygiene protects the rest of your mouth.
Gum Disease Stages and Why Early Treatment Matters

Gum disease has three main stages. Gingivitis is the earliest and mildest stage. It involves gum inflammation but no bone loss. The next stage is mild to moderate periodontitis, where the bone begins to recede. This stage is no longer reversible. Finally, severe periodontitis causes significant bone loss and tooth mobility.
Early treatment matters because gingivitis is the only stage that can be reversed completely. Treating problems early prevents long-term damage.
Gingivitis vs Periodontitis Around One Tooth
Localized gingivitis affects only the gums. The bone stays healthy. Localized periodontitis, however, affects both gums and bone. The early signs may look similar, but deeper pockets and bone loss show that the disease has progressed. If you feel the tooth becoming loose or if the gum pulls away significantly, it may be periodontitis. A dentist must evaluate the tooth to determine the correct diagnosis.
Foods, Habits, and Lifestyle That Make Gingivitis Worse
Sugary foods feed plaque bacteria, increasing inflammation. Sticky snacks cling to the tooth surface and attract more bacteria. Smoking or vaping reduces blood flow to the gums, slowing healing. Stress weakens the immune system and makes it harder for the body to fight infection. Poor sleep and dehydration also contribute to gum problems.
Improving diet, hydration, and lifestyle habits helps the gums recover faster.
Case Studies: Real Examples of Localized Gingivitis
Many patients develop gingivitis around only one tooth due to simple reasons. One patient experienced gingivitis around a lower molar because food kept getting trapped between the molar and a crooked neighboring tooth. Another patient developed inflammation around a single front tooth because they brushed too aggressively and caused gum recession, making plaque easier to collect in that area.
A third patient experienced localized gingivitis around a tooth with an old filling that had a small gap. Bacteria collected inside the gap, causing inflammation. All these cases show how quickly localized gingivitis can develop and how easily it can be reversed with proper care.
Tips to Prevent Gingivitis from Returning
Preventing gingivitis requires consistent oral hygiene. Brushing along the gumline removes plaque and prevents inflammation. Flossing daily removes trapped food that brushing cannot reach. Using mouthwash strengthens the gums and reduces bacteria. Regular dental cleanings every six months prevent tartar buildup. A healthy diet supports gum health, while staying hydrated helps maintain saliva flow.
Creating a routine and sticking to it prevents gingivitis from returning.
When to See a Dentist
If gum bleeding continues for more than a few days, you should see a dentist. Persistent swelling, redness, or pain around one tooth is a sign of inflammation. If the gum recedes or the tooth feels slightly loose, professional evaluation is necessary. Waiting too long can lead to more serious problems. A dentist can quickly diagnose and treat the condition before it spreads.
Myths and Facts About Gingivitis in One Tooth
One common myth is that gingivitis must affect the whole mouth. In reality, it often starts in one small area. Another myth is that gum bleeding is normal. Bleeding gums are always a sign of inflammation. Some people believe that brushing harder helps, but this actually irritates the gums more. Gentle brushing with proper technique is more effective.
Knowing the facts helps prevent misunderstandings and promotes better oral health.
Tips to Manage and Prevent Gingivitis in One Tooth
If you have gingivitis in only one tooth, the most important tip is to clean that area very carefully every day. Many people brush quickly and miss the same spot over and over, which allows plaque to build up and irritate the gum. Spend extra time brushing gently along the gumline of the affected tooth and make sure the bristles reach all sides. Using soft and slow movements helps remove plaque without hurting the gum further. Flossing around the tooth every day is also extremely important because food and bacteria often hide between teeth where the toothbrush cannot reach. When you floss, guide the floss gently under the gumline to clean away buildup and stop inflammation from getting worse.
Another useful tip is to rinse your mouth with warm salt water two to three times a day. Salt water reduces swelling, kills harmful bacteria, and helps the gum heal faster. It is safe, natural, and effective. Drinking more water throughout the day also supports healing because it helps keep the mouth moist and washes away food particles that can irritate the gum. If the tooth has a deep space where food gets trapped, consider using an interdental brush or a water flosser. These tools clean areas that regular floss sometimes cannot reach and prevent plaque from collecting around the affected tooth.
If you notice that brushing causes pain or bleeding, avoid brushing harder because it will only make the gum worse. Instead, use a soft-bristled toothbrush and gentle movements. Sometimes, switching to an electric toothbrush can help because the vibrations clean the gumline more effectively with less effort. Another helpful tip is to avoid sugary snacks and sticky foods while the gum is healing. These foods feed bacteria and increase plaque buildup, making gingivitis worse.
If the gingivitis is caused by a rough filling, crowded teeth, or a dental restoration that collects food, you should visit your dentist. They can adjust the filling, clean the area more deeply, or suggest solutions to prevent food from getting stuck again. Regular dental cleanings every six months are also essential because professional cleaning removes tartar that brushing and flossing cannot remove at home. Following these tips daily helps reverse gingivitis quickly and protects the rest of your mouth from inflammation.
Conclusion
It is absolutely possible to have gingivitis in only one tooth. Localized gingivitis is common and often caused by plaque buildup, food trapping, misaligned teeth, or poor cleaning habits. Early signs include redness, swelling, and bleeding around one specific tooth. With proper care, localized gingivitis is reversible, but ignoring it can lead to more serious gum disease. Understanding the causes, treatment options, and prevention strategies helps protect your oral health and prevents gum disease from spreading.
FAQ
Can gingivitis affect just one tooth?
Yes, this is called localized gingivitis and often happens where plaque collects more on one tooth.
What causes gingivitis in only one tooth?
Poor oral hygiene, food trapping, misaligned teeth, or a rough filling can cause inflammation around a single tooth.
How can I tell if only one tooth has gingivitis?
Look for redness, swelling, bleeding while brushing, or tenderness around that specific tooth.
Can gingivitis in one tooth spread to others?
Yes, if untreated, bacteria can spread and cause inflammation in nearby teeth.
How do I treat gingivitis in just one tooth?
Gentle brushing, daily flossing, rinsing with salt water, and professional cleaning usually reverse it.
How long does it take to heal gingivitis in one tooth?
With proper care, mild gingivitis can improve in a few days to two weeks.
Can I prevent gingivitis from returning to one tooth?
Yes, regular brushing, flossing, professional cleanings, and healthy habits help prevent recurrence.
When should I see a dentist for one-tooth gingivitis?
If bleeding, swelling, or tenderness persists despite good oral care, visit a dentist promptly.

Pingback: How Long After Tooth Extraction Can I Use A Straw
Pingback: What Are Tooth Gems